Back-up version ~ Art & Science of Modern Midwifery in California Feb 11, 2018 @ 6:45 pm
tinyurl.com/ybvde6cx
Safe, cost-effective Childbirth in the 21st Century
Healthy childbearing women and their babies are always safer when the mother-to-be receives regular prenatal care during pregnancy and is cared for by a trained and experienced birth attendant throughout active labor, birth of her baby, and the immediate postpartum-neonatal period, initial breastfeeding and follow-up care for both new mother and new baby for a minimum of six weeks after the birth.
That’s exactly what California Licenced Midwives are trained, licensed, equipped to do.
The California Licensed Midwifery Practice Act of 1993 (LMPA)
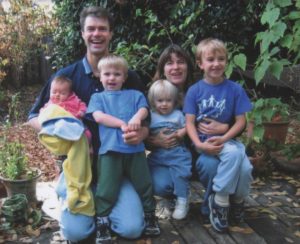
Four midwife-attended birth, 1st one in the hospital, and the next three as planned home births, baby #4 caught by dad as just as the midwife arrived (note dad’s big grin!) ^O^
The Licensed Midwifery Practice Act was passed unanimously by the California Legislature in 1993. Since then, approximately 50,000 families in California have had a midwife-attended spontaneous vaginal birth in out-of-hospital location. Every year more than 4,000 healthy pregnant women in our State seek alternative forms of maternity care from licensed midwives. In 2016, more than 3,000 babies were born in a non-medical setting (birth centers and family residence) under the care of California Licensed Midwives.
Professional midwives are “educated observers with emergency response capacity”. We watch, look and listen for a living, sitting quietly on the sidelines but always able and ready to spring into action if or when the need arises. Should an unexpected medical problem occur during pregnancy or childbirth, midwives are trained as first-responders, able to provide effective emergency interventions and when necessary, refer or transfer mother or baby to medical services.
This reduces risks during pregnancy, and the frequency and severity of preventable childbirth complications, making normal childbirth in healthy women both safer and more cost-effective. Midwives also provide emotional and social support for new parents in the weeks following the birth.
The current prematurity rate in the US is approximately 11% but less than 2% for women who received maternity cared from Ca LMs between 2007 and 2016.
 The Cesarean rate in the US is currently 32%, but for women who gave birth under the care of Ca LMs during those years, it’s less than 10%. **Licensed Midwives Annual Report (LMAR-2007-2016). Since 49% of all hospital births in the State are reimbursed by MediCal, these lower rates of prematurity and surgical delivery associated with the services of licensed midwives save California taxpayers many millions of dollars every year.
The Cesarean rate in the US is currently 32%, but for women who gave birth under the care of Ca LMs during those years, it’s less than 10%. **Licensed Midwives Annual Report (LMAR-2007-2016). Since 49% of all hospital births in the State are reimbursed by MediCal, these lower rates of prematurity and surgical delivery associated with the services of licensed midwives save California taxpayers many millions of dollars every year.
- cultural traditions
- strongly-held religious beliefs
- economic issues
- personal preference
 These families are hoping to avoid to the highly medicalized management of normal childbirth in the US, which they experience as similar to trying to give birth naturally in a busy ICU, lying in bed on their back while hooked up to IVs lines and fetal monitor leads, strangers going in and out, and the rest of their family standing out in the hallway, waiting for the baby to be born.
These families are hoping to avoid to the highly medicalized management of normal childbirth in the US, which they experience as similar to trying to give birth naturally in a busy ICU, lying in bed on their back while hooked up to IVs lines and fetal monitor leads, strangers going in and out, and the rest of their family standing out in the hallway, waiting for the baby to be born.  Tell Legislators to Vote for Stepping Stones, not Stumbling Blocks
Tell Legislators to Vote for Stepping Stones, not Stumbling Blocks
~ The Scientific Art of Midwifery, its History and its Future ~
The traditional role of midwives is:
“an educated observer with emergency response capacity”.
The midwife’s primary duty is to safeguard the normal physiological process while monitoring the well-being of mother and unborn baby. Midwives respond as the need arises, always being careful not to unnecessarily disturb or interfere with the normal biology of spontaneous childbirth as long as things are progressing normally.
This ‘eyes-on, hands-off’ quality of care describes a professionally-educated and clinically-experienced midwife who is physically present during active labor and able to watch and listen carefully and respond appropriately as the need arises.
This defines physiologically-based care as provided to healthy women with normal term pregnancies.
Historically, the presence of a trained midwife has always made childbirth orders-of-magnitude safer for laboring women and their unborn, and newly-delivered mothers and their newborn babies.
However, it is equally true that prior to the development of modern medical science, neither midwives or doctors were able to detect problems early on, before they became complications, and if a serious complication occ urred during or immediately after childbirth, obstetrical medicine had little to offer.
urred during or immediately after childbirth, obstetrical medicine had little to offer.
But early in the 20th century, it became possible to combine the time-tested methods of physiologic childbirth with the best advances in obstetrical science, to create (at least in theory) the best of both worlds.
The 20th-century marriage of Traditional Midwifery and Modern Medical Science
The scientific practice of modern medicine, and the incredible ‘medical miracles’ for which it is rightfully famous, originated with the new scientific ability to prevent bacterial contamination (germs and other pathogens) when performing medical and surgical procedures and to drastically reduce cross-contamination infections in hospitalized patients. Before these new discoveries, the high bio-hazard level of hospitals made them extremely dangerous — a place to avoid if at all possible.
So it’s fitting that modern maternity care also traces its history back to the discovery of the Germ Theory of infectious disease in 1881, and the risk-reduction strategies (principles of antisepsis) developed by the British surgeon to Queen Victoria, Sir Joseph Lister. This consisted of hand-washing, the use of disinfectants and germicides and surgical sterile techniques used during invasive procedures (such as vaginal exams during labor) and operations, including forceps deliveries and invasive medical procedures sometimes associated with obstetrical care.
Horray for modern biological sciences!
 What we now refer to as “maternity care”, which includes the new invention of prenatal care, wasn’t developed until early in the 20th century. The purpose of maternity care is to preserve the health of already healthy childbearing women. Mastery in this field means bringing about a good outcome without introducing any unnecessary harm or unproductive expense. In the US, 90% of women who become pregnant every year are healthy and at least 70% are still healthy and enjoying a normal healthy pregnancy with a single fetus in a head-down position nine months later.
What we now refer to as “maternity care”, which includes the new invention of prenatal care, wasn’t developed until early in the 20th century. The purpose of maternity care is to preserve the health of already healthy childbearing women. Mastery in this field means bringing about a good outcome without introducing any unnecessary harm or unproductive expense. In the US, 90% of women who become pregnant every year are healthy and at least 70% are still healthy and enjoying a normal healthy pregnancy with a single fetus in a head-down position nine months later.
 The development of prenatal care in the early 20th century allowed professionally-trained midwives and doctors, for the first time, to routinely risk-screen pregnant women at each antepartum visit. This included lab work to see that the mother-to-be wasn’t anemic or infected with hepatitis or a sexually-transmitted disease.
The development of prenatal care in the early 20th century allowed professionally-trained midwives and doctors, for the first time, to routinely risk-screen pregnant women at each antepartum visit. This included lab work to see that the mother-to-be wasn’t anemic or infected with hepatitis or a sexually-transmitted disease.
The pregnant woman’s blood pressure and urine were regularly checked for evidence of pre-eclampsia or diabetes, while the unborn baby’s growth, position, and heart rate were also monitored. This preventative care allowed small problems to be detected and corrected before they became serious complications. Equally important, it helped to identify women with serious medical conditions, such as heart or kidney disease, or high-risk pregnancies so they could be referred to an appropriate medical specialist.
During the 20th century, there has been a steady improvement in maternal-infant outcomes around the world. Many wrongly assume these improved outcomes were was the result of highly-medicalized care for healthy women in the world’s richest countries, particularly the US.
 However, these good outcomes turn out to be the result of an improved standard of living, general access to medical care and preventive use of people-intensive, low-tech maternity care. This describes the prophylactic use of eyes, ears, hands and knowledge base by maternity care professionals, who are able to screen for risk and refer for medical evaluation as needed.
However, these good outcomes turn out to be the result of an improved standard of living, general access to medical care and preventive use of people-intensive, low-tech maternity care. This describes the prophylactic use of eyes, ears, hands and knowledge base by maternity care professionals, who are able to screen for risk and refer for medical evaluation as needed.
This is the best ‘medicine’ for normalizing childbirth in a healthy population.
The story behind the 1993 Licensed Midwifery Practice Act (LMPA)
The California Licensed Midwifery Practice Act was introduced in 1993 by Senator Lucy Killea specifically to reduce the risks that pregnant women and their unborn/newborn babies face when the mother-to-be does not receive quality maternity care and associated complications including premature births and the dangers of unattended births.
Whether planned or unplanned, not having prenatal care and not having a trusted skilled birth attendant present during labor and birth drastically increases the danger to mothers and babies both.
Lack of prenatal care is associated with a dramatic increase in the rate of prematurity. The cost of caring for premature babies can be as much as a million dollars per infant and often includes expensive long-term disabilities. Treatment of newborns with respiratory-related difficulties, which is a major problem for premies, is the *very most expensive* type of hospital care — even more expensive than treating spinal cord injuries and 3rd-degree burns.
More than half of the hospital expense for pre-term babies is billed to the State’s MediCal program. Under dire circumstances, even high-income families come to depend on the State to pay for neonatal intensive care when their own private insurance maxes out. Unfortunately, the problems associated with a premature birth do not end when the baby comes home from the hospital. While the negative effects of pre-term birth fall heaviest on parents and child, there are also expensive downstream problems for our schools and other costs to society.
As for the risks of unattended birth, they are obvious and also expensive.
The Legislative Intent of SB 350 was to mitigate these problems by better serving the needs of families who couldn’t find afford conventional maternity care and/or wanted to avoid the highly medicalized and interventive hospital care. These families were seeking safe and lawful alternatives, including care by midwives trained to support the physiology of normal childbirth in a non-medical setting — the family’s home or free-standing birth centers staffed by professional midwives and family practice physicians.
Why Nurse-Midwifery Was Not an Answer

Certified Nurse-Midwife, Kate Bowland (standing) & provider of planned home birth services in Santa Cruz County for 45 years (Yea Team!)
At that time (1993), California law only legally recognized the practice of certified nurse-midwives (the Nurse-Midwifery Act of 1974). However, CNMs were only permitted to provide midwifery services if an obstetrician agreed to enter into a written contract to legally “supervise” them.
Unfortunately, the 1974 licensing law did not require that obstetricians provide supervision to this new class of midwife. As an additional disincentive to the practice of CNMs, the supervisory role of obstetricians meant they would be held liable for the care provided by the nurse-midwife if there was a malpractice suit.
For obvious reasons, the obstetrical profession has always seen midwifery as a competing profession and economic threat. So it was no surprise that most California obstetricians refused to take legal responsibility for one of their competitors. With rarest of exceptions, the few obstetricians who agreed to supervise a nurse midwife insisted that she only attend hospital births, which required the midwife to abide by obstetrical department protocols (instead of physiologically-based practices).

Standard obstetrical protocols for hospital delivery, with the mother lying on her back in an anti-gravitational position, trying to push her baby uphill, buried under sterile drapes, with the obstetrician, L&D nurses, a nursery nurse, several medical students and other hospital personnel looking on.
This unworkable law caused many frustrated families to seek out the services of lay midwives; when unable to locate a suitable birth attendant, they often opted for an unattended birth. This was such an obvious (and dangerous) problem that Jerry Brown, during his first term as governor (1975-83), became personally involved in supporting a new, non-nurse midwifery licensing law.
Governor Brown’s administration officially described the impasse over mandatory physician supervision as “structural barriers to practice” that prevented nurse-midwives from providing services to low-income women and families seeking alternative care. The California Department of Consumer Affairs, an agency of the executive branch, actively supported passage of a new midwifery-licensing law [AB 1896] as an independent discipline that was not controlled by the medical profession (as is still the case for California nurse-midwives).
 During this period of time, three midwifery licensing bills (AB 1896, AB??, SB??) were introduced and promoted by the Governor Brown’s office and Michael Krisman, Deputy Director of the Department of Consumer Affairs. There were a total of six failed attempts to pass a non-nurse (direct-entry) midwifery licensing law between 1976 and 1993.
During this period of time, three midwifery licensing bills (AB 1896, AB??, SB??) were introduced and promoted by the Governor Brown’s office and Michael Krisman, Deputy Director of the Department of Consumer Affairs. There were a total of six failed attempts to pass a non-nurse (direct-entry) midwifery licensing law between 1976 and 1993.
When this dismal record of overwhelming odds is taken into account, it was a bold move by Senator Lucy Killea to sponsor and actively promote SB 350 as an alternative solution to the problem created by the medical domination of all childbirth services.
The intent of SB 350 was to professionalize non-nurse midwifery and ultimately improve maternal-infant outcomes in California. The ancillary goal of the in the LMPA was also to reduce the State’s medical costs associated with a high rate of prematurity and childbirth-related complications resulting from a lack of access to maternity care and unattended births.
The LMPA passed the California Legislature unanimously and was signed into law by the governor on October 11, 1993. In 2016, more there were more than 400 midwives licensed in California under the LMPA and over 3,000 babies were born in non-medical settings (birth centers and family residence) under their care. **Licensed Midwives Annual Report (LMAR-2016)
PART 2 ~ An Important & Clarifying Amendment to the LMPA
The LMPA was first amended in 2000 by Senator Liz Figueroa. SB 1479 stated as a matter of California state law that childbirth was a normal aspect of biology and not a medical disease. SB 1479 legally clarified the characteristics of physiological management and the supportive, non-interventive practices associated with the community-based practice of midwifery, which is a non-medical (i.e. non-allopathic) discipline legally distinct from the allopathic practice of obstetrics.
By California law, the licensed midwifery model of care includes:
- Informed choice
- Continuity of individualized care
- Sensitivity to the emotional and spiritual aspects of childbearing
- Monitoring the mother throughout the childbearing cycle including
her physical, psychological, and social well-being - Providing individualized education, counseling, and prenatal care
- Continuous hands-on assistance during labor and delivery
- Postpartum support
- Minimizing technological interventions
- Identifying and referring women who require obstetrical attention

Hour-old baby boy being held by his new dad after being put in a “bunny bag” — a midwife’s invention that is a tiny sleeping bag made of baby blankets to keep newborns warm while being held by family members, who often have a hard time keeping the baby covered.
As amended in the year 2000, the LMPA formally acknowledged the right of essentially healthy pregnant women to exercise self-determination in regard to normal childbirth. This was an affirmative response by the Legislature to a legal issue raised by California Supreme Court in the Bowland Decision.
In 1976 the Bowland Court ruled that childbearing women had no intrinsic right to make decisions about the type of care they received during pregnancy and childbirth, noting that the California Legislature had “never gone so far” as to acknowledge that, as a class, healthy childbearing women in California had the right to choose “the manner and circumstances of normal childbirth”.
The Legislative Intent of SB 1479 rectified this oversight, acknowledging that, at least in California, noting that:
(b) Every woman has a right to choose her birth setting from the full range of safe options available in her community
(e) The midwifery model of care is an important option within comprehensive health care for women and their families and should be a choice made available to all women who are appropriate for and interested in home birth.
This provides legislative authority for traditional (i.e. non-physician) birth attendants and the choice by the parents of tradition/alternative (out-of-hospital) locations.
 The ‘Midwife Problem’ in California is NOT the midwifery practice act sponsored by Senator Killea, but LACK of access to high-quality maternity care and midwifery services for many women caused by inappropriate amendments to the LMPA by special interest groups
The ‘Midwife Problem’ in California is NOT the midwifery practice act sponsored by Senator Killea, but LACK of access to high-quality maternity care and midwifery services for many women caused by inappropriate amendments to the LMPA by special interest groups
Whatever people may think of community-based midwifery, they should be reassured by the following facts:
The public health problems surrounding normal childbearing in California is not a result of the care state-licensed midwives, but comes from the preventable danger to pregnant women and their unborn babies when they don’t get regular prenatal care and have unattended births.
The combination of no prenatal care and unattended labor and birth has 20 to 40-fold increase in maternal and perinatal mortality. One study of unattended births in a religious group identified 6 maternal deaths out of 344 births, or one maternal death out of 57 births. (Perinatal & maternal mortality in a religious group avoiding obstetric care – Am Jour Obst Gyne 1984 Dec 1: 150(7):926-31: ~ see abstract at end of this document)
However, the majority of unexpected problems associated with unattended childbirth can be prevented or successfully managed when the LMPA legally supports licensed midwives to:
- Provide regular prenatal care
- Physically examine and evaluate the health status of the pregnant woman and her unborn fetus prior to the onset of active labor (late pregnancy, very early labor), so those with complications can be prophylactically transferred to medical services
- Be present during the mother’s active labor, the birth of her baby and immediate postpartum-neonatal period and the 6-wk of follow-up care for both mother and baby.
But prior to passage of the LMPA in 1993, only two options were available to these families:
(a) “no care” – i.e. no prenatal care; unattended birth; delayed access to emergency medical services when needed
(b) a highly medicalized form of obstetrical care that is often experienced by laboring women and their families as similar to being in intensive care unit (ICU).
Midwifery Licensing and its Important Contribution to Childbearing Families
Passage of the LMPA in 1993 legally acknowledged and preserved the traditional art of midwifery. Over 400 California licensed midwives, whose role is that of have incorporated the historic quality of traditional midwifery care with the “best practices” of modern obstetrical-perinatal medicine.
If a medical problem should occur in a non-medical setting (home or birth center), midwives are scientifically trained first-responders able to provide effective emergency interventions, and refer or transfer mother or baby to medical providers whenever necessary. As noted earlier, this reduces risks during pregnancy, and the frequency and severity of preventable childbirth complications, making normal childbirth in healthy women both *safer* and more cost-effective.
Turning the Mother’s Shield into a Sword wielded by the Obstetrical Profession!
Unfortunately, the passage of AB 1309 in 2013 drastically reduced the scope of practice for direct-entry midwives. Previously, mandatory transfer to medical services only applied present-tense complications, which was a sensible solution that was embraced by parents, midwives and the medical profession alike.
However, the newest amendment to the LMPA calls for mandatory obstetrical consultation (even against the wishes of the childbearing woman) for identified risk factors. “Risks” describe the possibility of a complication in the future, but are not a complication itself that requires treatment. The obstetrician must then decide whether or not to permit the pregnant woman to resume her midwifery care; without this obstetrical approval, it’s illegal for the midwife to provide care. The consequences of this provision of the LMPA sometimes results in unattended births.
Ab 1308 also directly repealed the California Licensed Midwives Standard of Care and specifically negated our Standard of Care’s policy statement on the licensed midwife’s ethical duty to inform and recommend physician consultation in relation to all identified risk factors, and mother-to-be’s/parents right to self-determination, including to decline obstetrical referrals and evaluations.
AB 1308 eliminated the childbearing family’s right of self-determination with informed consent/refusal, while dramatically increasing the number of childbearing families that now don’t “quality” for midwifery services under the LMPA. I believe this provision is unconstitutional under both state and federal law.
As a result, an increasing number of essentially healthy women are being forced into what they believe is an unnecessary (and unwanted) hospitalization and highly-medicalized childbirth under obstetrical protocols.
A small but substantial number of these women had such a bad experience with a previous hospital birth (ex. unwanted induction or what they believe was an unnecessary Cesarean) that elective hospital birth is out of the question for them. If the local midwives aren’t legally allowed to provide care to them due to restriction introduced by AB 1308, they try to find a lay birth attendant or plan to have an unattended birth.
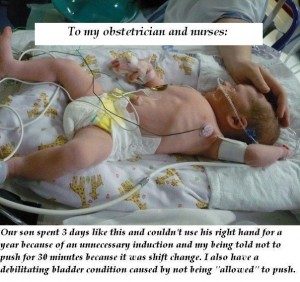 The adjacent photo is from a mother was who still upset and angry more than a year later about unnecessary intervention in her birth and iatrogenic complications for herself and her baby. She sent this picture of her newborn in the hospital’s NICU to her obstetrician and the L&D nurses, expressing her anger and disappointment.
The adjacent photo is from a mother was who still upset and angry more than a year later about unnecessary intervention in her birth and iatrogenic complications for herself and her baby. She sent this picture of her newborn in the hospital’s NICU to her obstetrician and the L&D nurses, expressing her anger and disappointment.
The original caption is to small to read, but it says:
“Our son spent 3 days like this and couldn’t use his right hand for a year because of an unnecessary induction and my being told not to push for 30 minutes because it was shift change. I also have a debillitating bladder condition caused by not being “allowed” to push.”
This directly negates many of the most important the contributions of Licensed Midwifery Practice Act, and the safeguards it provides by making it possible for a trained, experienced and equipped midwife to be present, and in most instances, able to prevent or successfully manage the unexpected problems associated with childbirth, especially as this applies to giving birth in out-of-hospital settings.
This must be fixed and soon!
 Reference #1 –Perinatal & maternal mortality in a religious group avoiding obstetric care – Am Jour Obst Gyne 1984 Dec 1: 150(7):926-31:
Reference #1 –Perinatal & maternal mortality in a religious group avoiding obstetric care – Am Jour Obst Gyne 1984 Dec 1: 150(7):926-31:
This control group consists of women with the same general health and demographic characteristics that are seen in the CDC birth registration data. This is predominately healthy, white, middle-class women who had economic access to all categories of maternity care providers and settings, but in this case, purposefully choose unattended births.
Data on this group of unattended home births came from Indiana state mortality statistics for a fundamentalist religious group that rejected all forms of medical care under all circumstances – no prior diagnosis or treatment of chronic medical problems, no risk-screening of mothers during pregnancy, no prenatal care, no trained attendant during childbirth and no emergency transfer of mother or baby with life-threatening complications to a medical facility – a situation similar to rural parts of the developing world.
Out of 344 births, the unattended group had 6 maternal deaths and 21 perinatal losses. The baseline mortality rate for unattended childbirth was one maternal death per 57 mothers or MMR of 872 per 100,000 live births (92 times higher than Indiana’s MMR for the same period) and one perinatal loss for every 16 births or PNM rate of approximately 45 per 1,000.
 Rosanna — here is the Tiny URL for this document. https://tinyurl.com/ybvde6cx
Rosanna — here is the Tiny URL for this document. https://tinyurl.com/ybvde6cx
You can use it for the CALM Google group if you so choose.
I have parts 2, 3 and 4 in draft form. They include the monkey-wrench of AB 1308, a longer, more history of mfry legislation in California, and why AB 1308 is unconstitutional (comparison btw ACOG Ethical Policies #166 and #214 and the MBC’s strike-thru of our standard of Care statement on the midwife’s duty to inform/warn and recommend physician consultation and mother’s/parents right to self-determination, including to decline obstetrical referrals and evaluations.
However, I but didn’t post the rest of this material last September, because no one seemed interested. But I will do so in next week or so, and text you when they are available.
Associated Topic –> The Obstetrical Standard of Care in the US – Historically Illogical, Fundamentally & Fatally-flawed